
Reference: Nguyen NM, Athota P, Flores A, Trease A, Meyer D, Singu VK, Krishnamoorthy C, Schaal VL, Bhakat R, Sualy K, Natarajan SK, Stauch K, Yelamanchili SV, Pendyala G. (2025). Comprehensive characterization of chronic midazolam exposure on neonates and long-term neurodevelopment. Mol Psychiatry.
This sedative disrupts brain development
Premature babies are born before their organs finish developing and often need medical help to do what their underdeveloped organs cannot accomplish. They may need a feeding tube to eat or a ventilator to breathe, and they are often given a sedative called Midazolam (MDZ) to make these medical procedures more comfortable. While MDZ may solve one problem, prolonged use can disrupt brain development and function, causing cell death, disruption in brain cell communication, and impairments in memory and learning (1, 2, 3). How long do these negative impacts last? Do these effects fade over time or do they persist? A recent study from researchers in department of anesthesiology at the University of Nebraska Medical Center in Omaha, Nebraska sought to answer these exact questions.
Early MDZ exposure impacts sociability during early adolescence
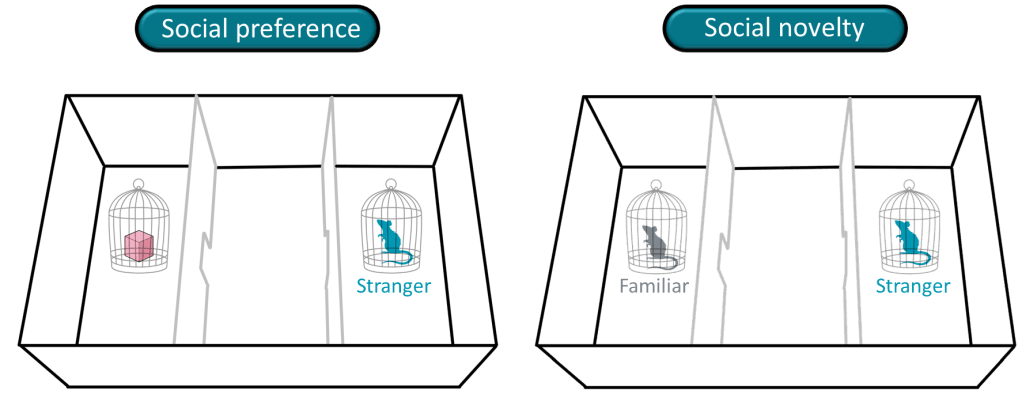
The team led by Dr. Pendyala, Professor of Anesthesiology and the Robert Lieberman Endowed Professor of Pain Medicine began by examining how early MDZ exposure affected brain development and behavior over time. Since rats share many of the same brain developmental processes with humans, they are often used in this type of research. The scientists gave rat pups either MDZ or saline, the control condition that does not impact brain development. Pups were then observed until they reached the human equivalent of young adulthood to see if MDZ affected social behavior and brain development. The scientists used a 3-compartment chamber to test the rats’ preference between an inanimate toy or an unfamiliar rat (social preference) and their preference between a familiar or unfamiliar rat (social novelty). In both tests, a sociable rat will spend more time with and interact more with the unfamiliar rat, but this was not the case for the rats that received MDZ. These sociability deficits were most evident during early adolescence and were not seen at later time points.
Early MDZ exposure affects normal brain processes
Next, the scientists conducted more tests to determine what other differences existed between rats given MDZ as pups and the ones that never received this sedative (saline controls). They were interested in the brain functions of the outermost part of the brain – the cerebral cortex – which is important for processes like memory and reasoning.
During childhood, the rats given MDZ as pups were lighter and their brains weighed less than the saline control rats. Additionally, during their childhood and young adulthood phases, these rats did not have the appropriate levels of growth factors, which are substances that regulate cell growth.
The scientists continued to find many more changes during young adulthood. Rats that received MDZ as pups showed increased inflammation in their brains compared to the saline controls. While the body typically triggers an inflammatory response to fight an infection or injury, some of the key players that initiate this process also take part in neurodevelopment. When scientists also discovered that the rats given MDZ as pups had low levels of dopamine, a chemical messenger important in motivation and feeding, they thought this could help explain why they gained more weight than the saline controls.
Additionally, MDZ caused lasting changes to proteins in the brain. Proteins are tiny molecules that work as “building blocks” to our bodies, providing structural support, transporting compounds, and transforming the food we eat. Young adult rats that were given MDZ as pups had changes to the functioning of relevant brain proteins, such as those associated with long-term memory, protein transport, and initiating the protein-making process. Fascinatingly, these rats also had changes in proteins that respond to stressed cells. When cells don’t have enough energy, they send out distress signals and the proteins that respond try to solve the issue by conserving energy and finding alternative energy sources.
What this means for care of premature babies
Can prolonged early exposure to MDZ have long term effects on the brain? Yes, it can change sociability, growth factors, dopamine levels, proteins, and inflammation. Still, more research is needed to understand the full extent of MDZ on neurodevelopmental effects. MDZ eliminates the discomfort that premature babies experience during necessary medical procedures so discontinuing it can have major consequences. With an estimated 1 out of 10 babies being born too early globally (4), it is especially important to find treatments that reverse these changes and alternatives to MDZ with less side effects on brain development. Having this information will help medical professionals make the best-informed decisions when taking care of premature babies.
Image Credits
- Cover photo: Canva
- Schematic of behavioral tests: Tracing and elements from Canva
Additional References
(1) Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K, Zorumski CF, Olney JW, Wozniak DF. (2003) Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. Feb 1;23(3):876-82. doi: 10.1523/JNEUROSCI.23-03-00876.2003. PMID: 12574416
(2) Nguyen NM, Vellichirammal NN, Guda C, Pendyala G. (2022) Decoding the Synaptic Proteome with Long-Term Exposure to Midazolam during Early Development. Int J Mol Sci. Apr 8;23(8):4137. doi: 10.3390/ijms23084137. PMID: 35456952
(3) Young C, Jevtovic-Todorovic V, Qin YQ, Tenkova T, Wang H, Labruyere J, Olney JW. Potential of ketamine and midazolam, individually or in combination, to induce apoptotic neurodegeneration in the infant mouse brain. (2005) Br J Pharmacol. Sep;146(2):189-97. doi: 10.1038/sj.bjp.0706301. PMID: 15997239
(4) Ohuma EO, Moller AB, Bradley E, Chakwera S, Hussain-Alkhateeb L, Lewin A, Okwaraji YB, Mahanani WR, Johansson EW, Lavin T, Fernandez DE, Domínguez GG, de Costa A, Cresswell JA, Krasevec J, Lawn JE, Blencowe H, Requejo J, Moran AC. National, regional, and global estimates of preterm birth in 2020, with trends from 2010: a systematic analysis. Lancet. 2024 Feb 17;403(10427):618. doi: 10.1016/S0140-6736(24)00267-8. PMID: 37805217.
